Background: Myeloid malignancies, including myelodysplastic neoplasms (MDS), chronic myelomonocytic leukemia (CMML), and myeloproliferative neoplasms (MPNs), pose significant morbidity and mortality for affected patients and can progress to acute myeloid leukemia (AML). Additional sex combs-like protein 1 ( ASXL1) is an essential epigenetic regulator with important biological functions. Damaging ASXL1 mutations are prevalent in myeloid neoplasms and are associated with poor prognosis and lower response rates with hypomethylating agents (HMA). In a phase I-II trial published by O'Connell et al. in 2022, patients with MDS and CMML previously exposed to HMA were treated with a combination of atezolizumab, an immune checkpoint inhibitor (ICI), and guadecitabine, an HMA. Bone marrow (BM) CD3+ T cells and CD34+ myeloid cells were tested for a panel of recurrent myeloid mutations. The two patients who achieved complete remission carried the ASXL1 mutation in both cell compartments. Furthermore, the ASXL1 mutation in T cells correlated with a significantly longer overall survival among the 27 patients tested, suggesting that ASXL1 mutations may prime T cells for response to immune checkpoint blockade. In this pilot study, we aim to determine the frequency of ASXL1 mutated T cells and the impact on T cells methylation profiles in patients with untreated, ASXL1 mutated myeloid neoplasms.
Methods:We included eight patients with known ASXL1 mutations detected by next-generation sequencing (NGS) in BM mononuclear cells . CD3+ T cells were isolated from the peripheral blood and separated by magnetic bead flow cytometry into CD8+ and CD4+ fractions. Sequencing libraries were generated using ClearSeq (Agilent) panel and were sequenced on MiSeq(Illumina). CD8+ T cell samples were aligned using a BWA aligner on Partek Flow (Partek) pipeline. Somatic calling was performed using the Strelka algorithm on Partek Flow. Each significant variant was confirmed by manual review using Integrative Genomics Viewer (IGV), and here we report the mutations present at a variant allele frequency (VAF) of at least 0.05 that correspond to those detected by NGS in the whole blood. In addition, DNA methylation studies were performed in the sorted T cells. We removed the loci with inadequate quality, and those associated with single nucleotide polymorphisms/age/sex chromatin. We performed methylation studies to identify differentially methylated locus and copy number variations.
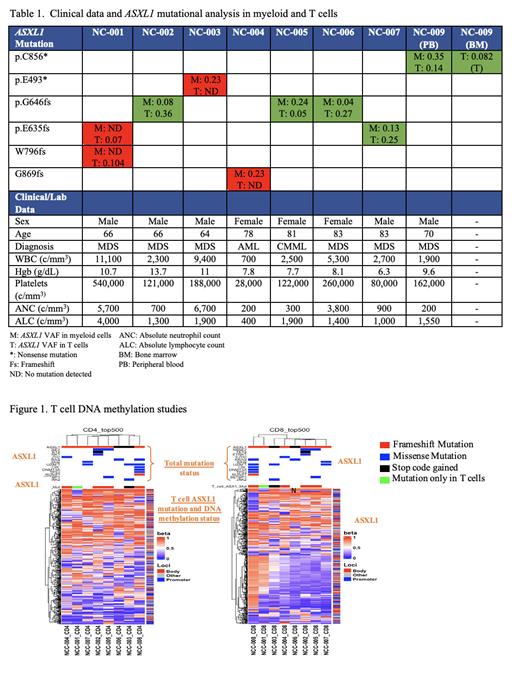
Results: We obtained peripheral blood samples from eight patients with ASXL1 mutated myeloid neoplasms detected by commercial NGS testing; aspirate was also obtained from a diagnostic BM biopsy in one patient. Table 1 shows patient demographics, characteristics and mutational analyses in both T and myeloid cells. Most patients were treatment-naïve, but one had been treated with HMA until 6 months prior to sample collection, and one patient had received cyclosporine for over 20 years for an undiagnosed autoimmune condition. T cells generated a mean sequencing coverage of 388x (min=341x, max=475x). ASXL1 mutated T cells were present in 50% (4/8) of the patients with myeloid ASXL1 mutations (Table 1). The median ASXL1VAF detected in T cells was 0.112. In 1 patient who also had a BM sample, the ASXL1 VAF in the T cells within the BM for this patient was 0.142, but only 0.082 in the peripheral blood. Methylation studies of peripheral blood T cell DNA did not delineate a clear difference between ASXL1 mutated and wild-type T cells (Figure 1).
Discussion: Approximately 50% of patients with ASXL1 mutated myeloid malignancies carry the same mutation in their T lymphocytes, which confirms the findings from a published report in a different cohort of patients, all of whom had been previously exposed to HMA. In that study the T cells were collected from BM aspirate whereas in this study they were from the peripheral blood. Unsurprisingly, the ASXL1 VAFis lower in T cells than in myeloid cells and may be lower in the peripheral blood than in the marrow, but this needs confirmation. Methylation studies did not detect unique profiles in samples with mutated T cells, but we were not able to isolate ASXL1 mutated T cells, so these data are less likely to represent the affected clones. Given the potential benefit of treatment with ICI in these patients, further characterization of ASXL1 mutated T cells including functional studies and receptor profiling is warranted.
OffLabel Disclosure:
Fernandez:Sobi: Membership on an entity's Board of Directors or advisory committees. Liang:Pangea Laboratory: Consultancy. O'Connell:Genentech: Other: Prior research support. Provision of drug for the study ; Astex Pharmaceuticals, Inc: Other: Prior research support. Provision of drug for the study .
Guadecitabine and atezolizumab

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal